Onychomycosis(Nail fungus) is a damage to the fungal infection of the nail plate and its surrounding structures: nail rollers, matrix (sprouts of the nail) and nail bed.It manifests itself by deformation and thickening of the nails, a change in their colors - the nails become white or yellow.
This disease is often found.According to some reports, the prevalence of onychomycosis in Europeans reaches 10-12 %and exceeds the known indicators of the past decade.It occurs 1.5 times more often in men, but they contact the doctor 2 -less often than women.Older people get sick more often, children are very rare.
The main problem in the treatment of the disease is that patients see a dermatologist long after the first symptoms have occurred.For this reason, the pathological fungus captures a large area and the treatment is delayed.
Pathogenic mushrooms can only be transmitted by a sick person.Very often an infection with a mushroom occurs in the family, since the source is not recognized in time and that do not adequate preventive measures are carried out.
Causes of the disease:Mostly direct contact with the patient or the objects used by him (shoes, clothing, carpets in the bathroom, washcloth, manicure supplies).Infection often appears when visiting gyms, bathrooms, saunas and pools.
The development of the disease is made possible by microses - cracks in interdigital folds that occur due to mattness, increased sweating, dry skin, poor drying according to water processes and flat feet.
Nail mycoses can also occur in the presence of simultaneous diseases of the endocrine system (diabetes, obesity, hypothyroidism), vascular diseases of the limbs (lack of veins, lymphostasis), immune disorders as well as when using antibiotics, corticosteroid and cytostatic drugs.As a result of the diseases mentioned above, the microcirculation of blood in the nail area is disturbed and natural immunity is reduced, which contributes to the development of a secondary infection.
Onychomycosis cause the following types of mushroom:
- Dermatophytes;
- Hefe -similar mushrooms of the genus Candida;
- Shape.
Depending on the type of pathogen, the penetration of a fungal infection and the clinical image differs, so that the therapy approaches are different.
The nails on the legs are affected by a mushroom 10 times more often than by hand.In most cases, dermatophytes cause the mushroom (for example Trichophyton rubrum).The remaining cases are most often caused by inconsistent forms (aspergillus, scopulariopsis, fusarium).
If similar symptoms are found, consult a doctor.Do not do yourself - it is dangerous for your health!
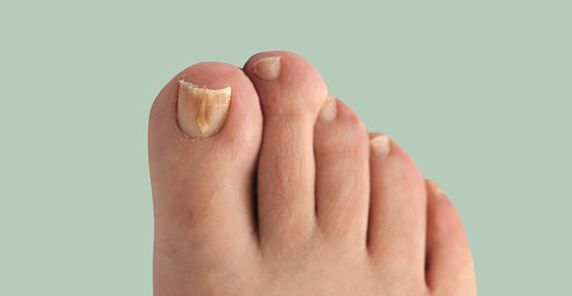
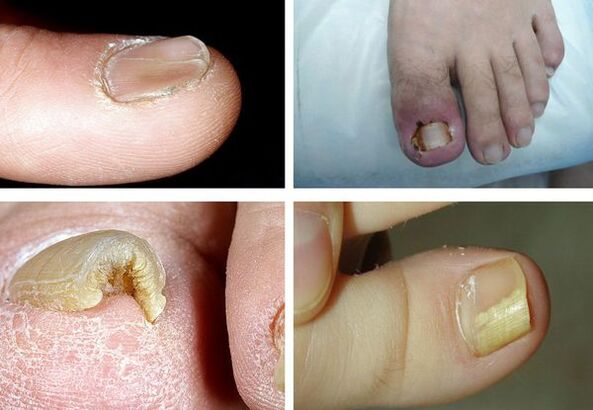
Symptoms of onychomycosis (nail fungus)
The longer the disease takes place, the more pronounced your symptoms become.The main signs of onychomycosis are:
- Dydromy - a change in the color of the nail to yellow, black, green, gray or brown (the type of color depends on the type of fungus);
- Onycholysis - separation of the nail plate from the box;
- Change of the thickness of the nail plate;
- Gapalonichia - a power of the thickness of the plate and its softening;
- Koylonichia - The nail looks concave, in the form of a teaspoon;
- Pahionichia - thickening of the nail plate, hypertrophy of the nail;
- Onichogrifosis - thickening, a change in the color of the nail plate, rolled up in the form of a bizarre;
- Change the thickness of the nail bed (hyperkeratosis - thickening of the nail bed);
- Change the surface of the nail plate: pits, furrows, coat of arms;
- Change the nail rollers and the surrounding skin (paronych - inflammation of the proximal nail roller).
It is important to note that not one of the symptoms is pathogen, i.e. clearly suitable for a certain pathogen.It is therefore impossible to determine this by symptoms - additional examinations are required.
Pathogenesis of onychomycosis (nail fungus)
The pathogenesis of the disease depends on how the fungus meets skin and nails.
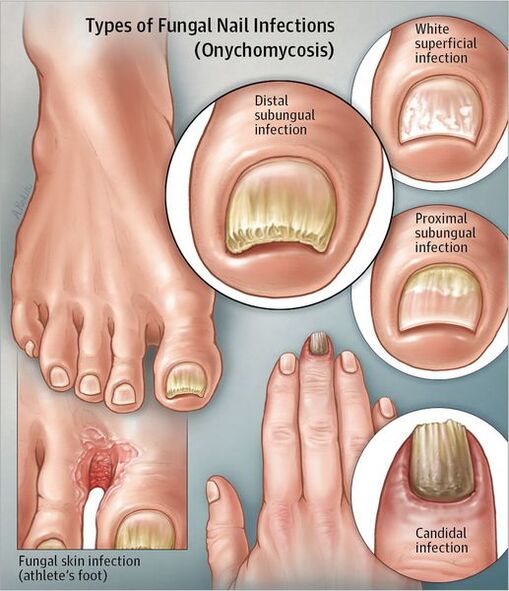
Distal U -Boat type:If the fungus is inserted through the skin in the area of the nail rollers or in the distal area, the infection is spread by the free nail edge in bed and further to the matrix.First of all, the nail plate cannot change, but later gradually from the nail bed due to hyperkeratosis and becomes yellowish.A thickening of the nail plate is gradually possible.
Superficial white type:When white focal points form on the surface of the nail, the entire nail plate occurs over time.The nail thickens, crumbles, gets a gray -brown color.In this case, the matrix and epithelium of the nail bed are not affected.There is no inflammation of the surrounding skin.
Proximal undergance type:The mushroom can spread from the skin and periological rollers to the nail plate and then to the matrix and reach the distal parts of the nail plate.Spots appear on the nail in the area of the hole and the nail bed, the nail plate is replaced.There is no pronounced inflammation of the nail bed or the matrix.
Total dystrophic type:The whole nail is affected.The proximal areas of the nail roller disappear or thicken so that the nail plate can no longer form and grow.
ExistedThe biophysical concept of the pathogenesis of onychomycosisWhat states that the disease confronted the two forces: a mushroom colony that grows towards the matrix, and the natural growth of the nail from the matrix to distal edge.Therefore, the growth rate of nails during onychomycosis is of crucial importance - the faster the nail grows, the earlier the healing comes.Perhaps this explains exactly what explains the little prevalence of the disease in children, since their nails grow faster than in adults and older people.
Classification and stages of the development of onychomycosis (nail fungus)
There is the following classification of onychomycosis:
- Distal u -boat;
- superficial white;
- Proximal underground movement;
- Totally dystrophic.
After the classification of 1970:
- Normotorophical: In the thickness of the nail, a yellowish and whitish colors, but the shape of the nail plate does not change, there is no U -boot -hyperkeratosis;
- hypertrophic:The nail plate becomes yellow, thickened due to a U -boat hyperkeratosis, breaks with jagged edges;
- Dystrophic:There is a thinning and removal of the nail plate from the nail bed with the formation of cavities.
Complications of onychomycosis (nail fungus)
The development risk increases with long existing onychomycosisdiabetic(Formation of trophic ulcers on the legs) andgangrenewhen the patient has diabetes or vascular diseases of the lower extremities.

In immunosupine conditions (primary and secondary immunodefinal) mushrooms can spread to the skin that spread internal organs and cause allergicization of the body.This can be manifested by rashes on the skin up to the development of bronchial asthma.
Diagnosis of onychomycosis (nail fungus)
Before you start the diagnostic procedure of onychomycosis, it must be explained how the material for the study can be properly installed (the patient does it independently or before diagnosis nails).Before the fence of the material for the study, it is necessary to treat the nail plate with 70 % alcohol so that there is no obstruction of other bacteria.
The method for collecting material varies depending on the shape of onychomycosis:
- Superficial form- Make a scratch out of the nail plate;
- Distant form- A scratch from the nail bed and a piece of the nail plate is necessary;
- Proximal U -boot shape- The material is harvested by a drill or a biopsy of the nail or a scratch from the nail bed.
The fastest method for determining pathological mushrooms is in the nailmicroscopy.Technology: The examined material is treated with a solution from alkali for the resolving of keratin.In order to make the mushroom threads better, the alkali ink is added.Next, examine the resulting drug under a microscope.
This research method is the fastest and most objective.The sensitivity is up to 80 %.One of the disadvantages of the method is the fact that it is impossible to determine the type of pathogen when using it.
Bacteriological sowing: is an additional method for diagnosing onychomycosis.The material is sown in a special environment and the result is interpreted under a microscope after 2-3 weeks.With this method you can define the type of pathogen.This helps to determine the tactics of the treatment and the selection of medicinal products through sensitivity.However, the disadvantage of the study is that it takes a lot of time and its sensitivity is only 30-50 %.
biopsy: With the help of a scalpell and using anesthesia, a nail and a nail bed are cut off.The material is immersed in a formal hydration solution and sent to the laboratory for histological examination.The advantages of this method are highly sensitive and enable you to determine the presence of a pathological mushroom in the material.
Disadvantages: It is impossible to identify the pathogen and to determine the life capacity of microorganisms, the high costs and complexity of the method.
Genod diagnosis: Molecular biological research method (PCR).This is one of the new and highly sensitive methods for diagnosing onychomycosis with the help of this, the DNA of the pathogen is revealed.It is recommended to introduce this type of diagnosis in those medical institutions with PCR laboratories.At the moment, test systems have to identify dermatophytes and molds, and only plan the introduction to the laboratory.With the method you can determine the type of pathogen and its sensitivity of 80-90 %.Disadvantages - high costs, inaccessibility, lack of technological standards and the complexity of the execution.
More and more doctors are being introduced to the practiceDermatoscopy.With this method you can rate a change in the color and structure of the nail, the condition of the surrounding structures.With dermatoscopic examination, you can evaluate the depth of the damage to the nail plate more precisely and correctly calculate the index of the severity of onychomycosis.
Treatment of onychomycosis (nail fungus)
There are different types of treatment for onychomycosis:
- Local therapy.
- System therapy.
- Combined therapy.
- Correction therapy.
Local therapyIt is about applying medication on the nail plate and the nail rollers.Indications for local therapy:
- Limited form of damage to the nail plate.
- There are contraindications for the appointment of systemic medicines: hypersensitivity, liver disease, kidney function, pregnancy, lactation.
The advantages of this therapy are that high concentrations of a therapeutic means are formed on the surface of the nail, which does not penetrate into the blood circulation.There are no side effects of using antifungals - nausea, a decrease in appetite, abdominal pain.The disadvantage of the method is that the medical substance does not always fall into the habitat of the pathogen, especially if the mushrooms are in the nail bed or in the nail bed or in the matrix.This in turn can lead to an inefficiency of the treatment.This type of treatment is very time -consuming because it must remove the affected part of the nail before using the drug.
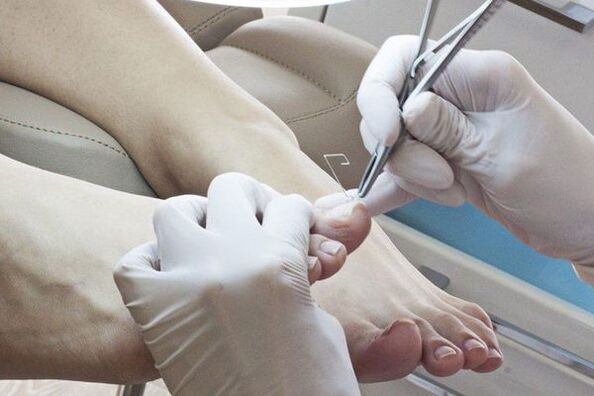
Possibilities for removing affected nails:
- Mechanical distance with files, nipper or drills.
- With the help of keratolytic plasters.Before applying a keratolytic pavement, the skin around the nail is sealed with a patch, a patch mass (urea with salicylic acid) is applied at the top and sealed with an adhesive plaster.The patch mass is changed every 2-3 days.After each distance, the affected part of the nail is removed mechanically.
- Surgical.This operation is very painful and traumatic, since the spray zone can be damaged when removing the nail plate, which leads to the growth of deformed nails.
After removing the affected nail plate, local antifungals are used.AntimicticsDifferentiate between the location:
- Applied to the nail: varnish;
- Apply on rollers: creams, ointments, solutions.
The most investigated instrument for local use is a 1 % solution to the drug group of the drug group, which has a proof of evidence in treatment on the basis of the coocranny meta-analysis.This tool has a water base that contributes to the better penetration of the antifungal substance in the destruction site.Lackien have a dehydrated basis that reduces the penetration of the drug into deep layers.Therefore, dermatologists take into account the use of varnishes unsatisfactory and more and more often prefer a water -based tool.
In order to obtain the result from local therapy, it is necessary to observe the treatment scheme.It is important that the patient is responsible, consistent and patient.The therapy duration can reach 12 months.
System therapyEnables the antifungal to penetrate the lesion through the blood, even if the nail bed and the matrix are affected.The high concentration of the drug remains in the lesion for a long time after the end of use.The disadvantages of this type of treatment are associated with the risk of side and toxic effects.
Indications for systemic therapy:
- Common forms of damage to the nail plate.
- The lack of the effect of local therapy (i.e. after six months of treatment of onychomycosis on the hands and 9-12 months of the treatment of onychomycosis of the feet there were no growing healthy nails).
To determine the treatment tactic, a clinical index is used by the severity of onychomycosis.It is used as a therapeutic standard in different countries in the world.
MedicationTo treat onychomycosis, you can classify as follows:
- Anti -Cikat - have an antifungal effect;
- Antiseptics - have both antifungal and antibacterial effects.They are rarely used, only if there are no other antifungals;
- Multi -components - In addition to an antifungals, other medicines such as anti -inflammatory anti -inflammatory drugs contain.
Medicine to prescribe drugs:
- Standard - daily administration of medicinal products during the prescribed treatment time;
- shortened - the treatment time is shortened, can be carried out or enlarged by conventional doses;
- Intermittent - treatment is prescribed in several short courses.The intervals between courses correspond to the duration of the courses.
- The pulse therapy treatment is prescribed in several short courses.The intervals between courses are larger than the duration of the courses.
Antimyotika are divided into an active substance:
- Triazole;
- Alllamine;
- Morpholine.
System therapy is currently being usedOnly third generation medication.
With combined therapyLocal and systemic treatment are carried out at the same time.Combined therapy is used if it is necessary to increase the effectiveness of systemic therapy and reduce the treatment periods.
Correction therapy(Treatment of accompanying diseases): In order to select a treatment scheme, the general somatic state of the body must be assessed.Diseases such as circulatory diseases in the limbs can reduce the access of the antifungal to the lesion.Therefore, medicines that improve fabric trophy are prescribed.
Due to the toxic effects of systemic antifungals, it is necessary to exclude liver diseases and to prescribe hepatoprotectors if necessary.
Forecast.prevention
The earlier the patient contacts the doctor with signs of fungal nail läsions, the faster the disease is healed and the nail plate restored.With long existence of processes with the edging of the entire nail, the treatment of onychomycosis can be long, but recovery often occurs under all recommendations.For contraindications for systemic therapy, long -term support with local drugs is required.
For preventionIt is necessary to comply with the rules of personal hygiene and reduce the possibility of a re -in -in function:
- Try to wear comfortable and high -quality shoes (to prevent increased sweating of the legs);
- It is recommended to change socks and tights every day.
- Use only individual shoes.Those who are treated onychomycosis must be treated at least once a month during the entire treatment time and after their end at the beginning of treatment.
- If necessary, use antiperspirants for the legs.
- Use individual nail care set (scissors, sawing);
- Before and after visiting public places (pool, bathroom, sports hall), use antifungal external products (sprays, cream and pens);
- Determination of the source of a fungal infection in the family and treated at the same time.
It is recommended to regularly carry out the antifungal processing of personal objects, shoes, baths, floors and carpets.For these purposes you can use a 40 % solution of acetic acid, 1 % alcohol solution of antiseptic (prescription prescription by a doctor) and use solutions for disinfection.Lingerie can be cooked in 1-2 % of the soap liner solution for 20-30 minutes and ironed at maximum temperature.




















